




36%
Members 0-18 years old
(includes Medicaid, behavioral health, dental and Tribal members)
$17.9 million
Amount we reinvested in Oregon communities in 2021
1,003
Number of employees in the CareOregon family
(as of 12/31/2021)
Our mission
Inspire and partner to create quality and equity in individual and community health


We act to benefit others and our communities
We embrace challenges and live our purpose
We're empowered to indentify and make changes
We jointly commit to exceptional achievements
We're curious, going beyond the status quo
We respect, support and cooperate with others
We treat everyone fairly and without bias
We respect and embrace individual differences

Through grants, language interpreters and outreach staff, CareOregon supported organizations that put together culturally specific, party-like clinics for vaccine-hesitant populations. Did they work? “So hugely,” said Caroline Pope, Member Engagement Supervisor at CareOregon. “The community was embracing any kind of fun.”


After CareOregon designated $96,000 for Jackson Care Connect’s “provider wellness fund,” our staff partnered with Rogue Food Unites to put together and deliver provision boxes to frontline workers. The care packages served a dual purpose: Thank workers in health care and social services. And support small businesses by featuring locally produced foods. “We wanted to provide nourishment through healthy, delicious food,” said Sam Watson, Community Health Manager – and a night off from cooking.


When a teammate referred a female Elder to Behavioral Health Care Coordinator Toby Brooks – an Alaska Native himself – he knew the right approach: Sit back. Listen. Don’t interrupt. The Elder confided to Brooks she feared stigma if she got therapy. Nine months of supportive calls later, the Elder was ready to take that step. Thanks to telehealth, Brooks could match her with a Bend therapist who’d grown up among Tlingit people and was versed in trauma-informed care.


Accessing mental health care was difficult even before COVID-19. Then the virus hit, thinning provider ranks from illness and burnout. “We saw a worsening of conditions among people with substance abuse and other mental health issues,” said Amit Shah, MD, Chief Medical Officer. “We needed to find out what we could do to preserve access to care.” CareOregon’s answer was unique among the state’s 16 coordinated care organizations: a first-ever emergency fund for mental health care providers. This lifeline helped keep doors open in seven of Oregon’s most populous counties.
CareOregon is in the midst of planning a multi-year investment to improve and expand mental and behavioral health care. But as the pandemic entered its second year, provider services eroded alarmingly.
“We have a plan for transformation, but we are in a crisis right now,” said Jill Archer, Vice President of Behavioral Health Services. “We can’t transform a decimated system where we can’t even get people in for care.”
CareOregon’s Board of Directors asked what could be done immediately. CareOregon took that question to providers, who greeted it with surprise and pleasure. “We can’t believe you’re asking,” one responded.
After the board approved the $7.5 million emergency fund in April, staff reviewed proposals from behavioral health providers. We moved quickly, sending most of the funds to providers’ hands by the end of July (with about $700,000 to be disbursed in 2022). Grants ranged from $15,000 to $500,000, paid as recruiting and retention bonuses and more.
Rural areas like Medford and Oregon coastal cities used grants to pay first and last months’ rent in an effort to draw mental health care professionals who wanted to work there but couldn’t afford to relocate.
Investments from laptops to wellness activities increased worker productivity and satisfaction. Pay differentials helped those who work with more-complex patients.
Teaching trauma-informed care helped staff to better treat members; training them in stress management helped staff treat themselves better.
Providers who received grants serve nearly 85% of the highest-need Oregon Health Plan members in the Portland tri-county area, and Columbia, Clatsop, Tillamook and Jackson counties.
“The emergency fund kept providers and their finances stable,” said Shah. “Key partners didn’t have to close their doors.”

A $2.5 million investment from CareOregon enabled Portland Fire & Rescue to launch Community Health Assess & Treat (CHAT) in the bureau’s new community health division. The pilot program, which aims to improve equity and access, addresses a major gap in community health. In October, CHAT began a 12-month test of a novel approach with CareOregon members and others who call 911 for lower-risk medical concerns. These 911 calls are directed to the specially trained CHAT medics. They assess the community members face-to-face, provide prompt care and, if needed, guide them to other resources, including the Oregon Health Plan (OHP). The medics also offer a follow-up visit 24 hours later, and education about preventive care.
About a third of the medical calls to Portland’s 911 system are for low-risk medical needs. Before CHAT was introduced, all 911 calls typically got the same level of response: an ambulance and transport to an ER.
Now, two CHAT medics in an SUV respond to a portion of these lower-level calls. The program operates in downtown and outer Southeast Portland, where many such calls originate.
CHAT medics can deliver immediate care, devote the time to determine what further services are needed, then transition the individuals to that care – be it dental, urgent care or, in fact, the ER.
If the community members are insured, CHAT medics guide them on using their benefits, such as preventive care from a primary care provider or dentist. If they are uninsured, the medics help connect them to resources for enrolling in a health plan, including OHP.
Behind the scenes is a solution-focused partnership and a responsive, multidisciplinary team of CareOregonians committed to CHAT’s success. Throughout most of 2022, CHAT and CareOregon will continuously refine and evaluate the effectiveness of this less costly, flexible and more-personalized alternative to the classic emergency medical response.
“Up until now,” said Fire Chief Sara Boone, “we haven’t had a mechanism to allow us to spend the time needed to assess and treat community members on scene and connect them with appropriate care and resources.”
The pilot program’s goals align with health care’s Triple Aim: improve health outcomes, lower health care costs and improve member experience with the health care system.

In 2021, we awarded an unprecedented $17.2 million to community-based organizations, including our provider networks. CareOregon recognizes that a host of factors – known as social determinants of health – affects well-being. Our grant-making includes an eye for partnerships that positively impact these influences. A sampling of these supportive investments includes a Boys & Girls Club in an underserved neighborhood, health centers housed in two Clackamas County high schools, and a grant to boost the number of health care interpreters and their training.
Play ball, tackle academics, meet with mentors, tap into family supports. Boys & Girls Clubs go all out to put young people on the path to a great future, which made the Portland Metropolitan Area clubs a natural fit for CareOregon. In late November, we announced a 10-year, $2 million collaborative partnership with the Rockwood location, 454 SE 165th Ave. The newly renamed CareOregon Boys & Girls Club at Rockwood is right where we want to be; a higher percentage of residents in nearby ZIP codes qualify for the Oregon Health Plan than anywhere else in the state.
Through our Provider Emergency Relief fund, CareOregon invested $5 million in strengthening our provider network. This included health centers at two high schools in the North Clackamas School District; our $250,000 grant supported staffing. After two years of delayed health care, children’s need for health and wellness care is especially great, said Carol Keep, RN, of Clackamas County. Operated by the Clackamas County School-Based Health Center program, the new facilities opened in fall 2021 to serve students K-12. Physical health screenings and routine care, cleanings by a dental hygienist, and mental health services are offered, regardless of insurance or immigration status.
“At a time when many families are struggling to meet their basic needs, increasing access to no-cost health services at school is one way we are partnering with community to remove barriers so all families can be as healthy as possible.”
– Robert McConville, Vice President of CareOregon Metro
Good health care relies on patients and providers communicating well. With a $250,000 two-year grant to the Oregon Health Care Interpreters Association, CareOregon is helping build workforce capacity and clearer communication between care teams and English-learner members. The money is enabling current and prospective interpreters to complete training courses and undergo state credentialing – priorities of the Oregon Health Authority (OHA).
“Good communication creates the bond between patient and provider that promotes health awareness, timely access, treatment compliance and a healthy lifestyle.”
– James Mason, PhD, CareOregon Chief Equity, Diversity & Inclusion Officer

The pandemic changed everything about employee expectations, including at CareOregon. The company adopted long-term remote work and scheduling flexibility for all appropriate positions, accommodating the desire for work-life balance. “They also told us, ‘I really want a culture of belonging, so even if I’m working from home, I feel a part of my team and organization,’ ” said Chantay Reid, Vice President, Human Resources. To help meet those needs, the company instituted employee resource groups (ERGs) and a sabbatical program, and elevated personal and professional development into a strategic initiative.
After staff expressed strong interest, in early 2021 the company rolled out its program for employee resource groups. The five employee-led affinity groups are among the ways CareOregon is working to promote a diverse and inclusive environment, cultivate a sense of belonging, and support personal and professional development.
The idea of offering sabbaticals came from a CareOregon Board of Directors member who sits on the compensation committee; she suggested them as a means of strengthening retention, engagement and work-life balance. After exploring the possibility, leadership and the full board agreed, and set a January 1, 2022 program launch date. The first level of sabbaticals, available to those with five or more years’ tenure, pays 25% of salary for four to 12 weeks. The first sabbaticals are beginning July 2022.
HR’s Organizational Development and Learning team added breadth and depth to CareU, our online home for classes and leadership development programs such as Aspiring Leaders. The library of on-demand offerings includes subjects that range from leading a remote team to breathing exercises that reduce stress. Jonathan Weedman, Vice President, Population Health, led an especially timely live remote class: Resiliency 101. As employees at many organizations rethink their purpose and position, “it’s a critical course,” noted Mara Kershaw, Director, Organizational Culture and Development.
“The long-term employees know what the CareOregon in-person culture is like. The new employees don’t. How do we help them experience the culture – that, I believe, was part of retaining employees? It’s not the same trying to build that connection through a little square on the computer.”
– Chantay Reid, Vice President, CareOregon Human Resources
The company’s exceptional culture again won attention in an annual survey of workplaces. For the sixth year running, CareOregon was named by The Oregonian/OregonLive as a Top Workplace, based on the news organization’s survey of our staff. “That means,” says Reid, “our employees are declaring us an employer of choice.”
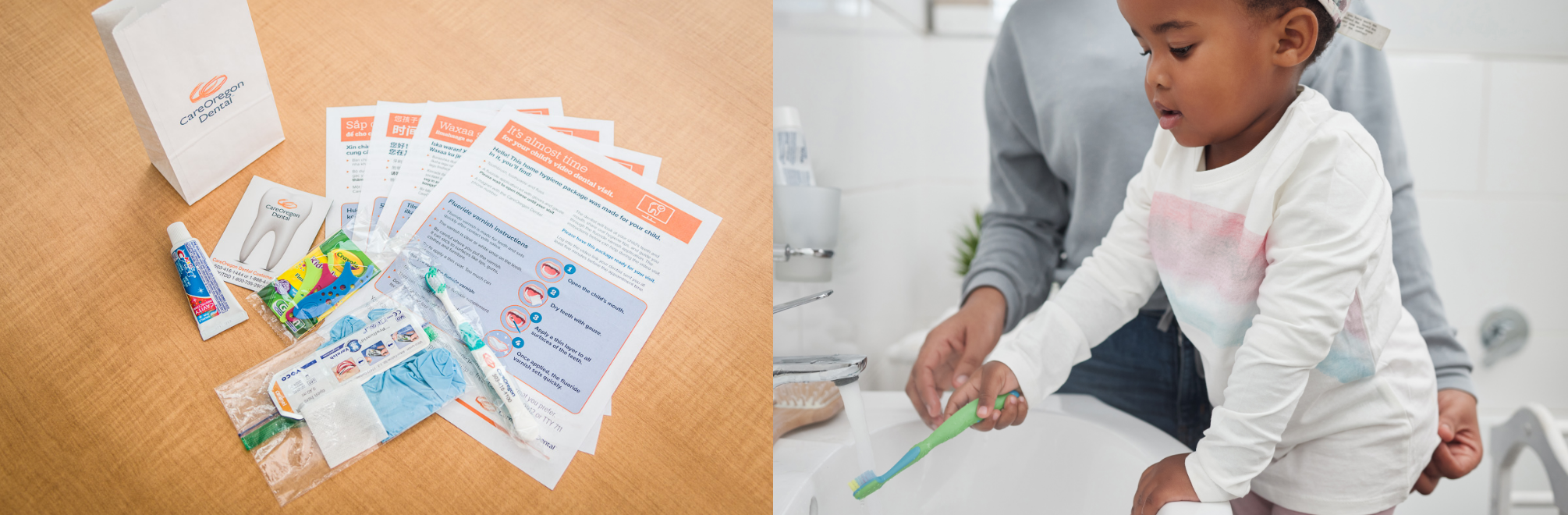
CareOregon Dental initiated a pilot preventive teledentistry program for children, enabling three dental partners — Clackamas Health Centers, Neighborhood Health Center and Virginia Garcia Memorial Health Center — to offer video dental appointments to members in the Portland area. The program aimed to increase members’ access to dental care and introduce a virtual option for seeing dental providers. CareOregon Dental provided dental partners with dental hygiene kits for young patients and their parents. Dental clinics sent 76 of these packages to families, pre-appointment, equipping them with guidance for video appointments, toothbrushes, toothpaste, floss and a fluoride application kit. During the teledentistry visit, dental staff employed motivational interviewing to review nutrition and oral hygiene instructions, and help parents apply fluoride varnish to their kids’ teeth.
When the COVID-19 pandemic began, adults and children alike had limited or no access to dental care. Even as clinics reopened, many families reported hesitation and anxiety about in-person visits. Meanwhile, some dental clinics and systems were slow to adopt video appointments and were only able to offer telehealth visits by phone.
A few months into the pandemic, CareOregon Dental helped some partners implement teledentistry triage and prevention services, and then developed the pilot program. For the first time, dental partners offered video appointments, gaining the experience they needed to continue the service long-term.
After the pilot’s completion in late 2021, CareOregon Dental met with dentists, hygienists and outreach staff to discuss key takeaways. They found that pediatric dental telehealth offers benefits to both members and dental clinics:
A second program phase will begin in mid-2022. The aim is to offer this preventive teledentistry model and learnings to CareOregon Dental’s provider network by end of the year.
“Being able to provide telehealth services focused on prevention for our younger patients has been an exciting new endeavor. We have been able to increase our reach to patient populations who may have been avoiding in-office visits for several reasons, and we believe we are giving these children and their parents an equally valuable service as the one they would receive in our clinics.”
— Shannon Eckes, Dental Hygienist, Neighborhood Health Center

When COVID-19 vaccines reached the public, the CareOregon family was ready to serve our members on multiple fronts. We provided accurate medical information, culturally appropriate care and language interpretation services. We worked with partners to support practical access to the vaccine – no matter an individual’s physical limitations or housing situation. Through partnerships and internal initiatives, we put great effort into fulfilling our commitment to vaccine outreach and equity. And we did this work with sensitivity to some communities’ longstanding mistrust of government guidance and the medical system.
During COVID-19, how to encourage high-risk members to get care, including vaccines? Using data, CareOregon’s enterprise-wide Population Health Partnership team ultimately decided to focus on three groups: pregnant members, medically complex vaccinated adults who were eligible for boosters, and vaccinated parents with unvaccinated children.
Along with the cross-departmental Rapid Response Team, staff devised a new approach of texting the targeted members to alert them that our staff would be reaching out soon with a personal phone call. For vaccinated parents, the team texted resources for accessing child vaccinations.
These efforts were among those in our COVID-19 High Risk Outreach Playbook, which the Institute of Medicaid Innovation honored as one of the top 25 projects nationally for addressing health inequities during the pandemic.

Equitable access to COVID-19 vaccines can call for more-tailored solutions than the mass vaccination events that took place across the state. Enter Columbia Pacific CCO, which in 2021 implemented a vaccination program with Columbia River Fire & Rescue. The goal: Vaccinate members in Columbia County who are homebound or have limited access to transportation.
The initiative grew out of an existing relationship. Columbia Pacific already contracts with the fire department; its community paramedic, Nina Kerr-Bryant, makes home visits in Columbia County to members who have chronic conditions. When the pandemic struck, Kerr-Bryant pivoted from providing care planning and education to vaccinating members who were confined to their home. She also provided other types of support, such as delivering medicine and monitoring blood pressure.
“This was a hyper-local effort to reach some of our most-vulnerable members. The fire department is respected at the local level, and that trust within the community helped reduce some vaccine hesitancy.”
– Bethany Pettinger, Population Health Specialist, Columbia Pacific CCO
Jackson Care Connect joined forces with community paramedics, public health and nonprofits on a pair of comprehensive efforts to help county residents overcome barriers to vaccination, ranging from misinformation to lack of mobility.
Our $15,000 grant to Mercy Flights allowed its Mobile Integrated Healthcare Program to expand into vaccinating homebound individuals – and reducing social isolation – as well as unhoused residents. The team also distributed hygiene kits each week in urban and rural areas to people without shelter.
Jackson Care Connect staff members co-chair the county’s Vaccine Equity Hub, part of the local Covid Response Equity Plan. With a unified voice, the hub supported initiatives that were community-based and culturally and linguistically responsive. They included a multicultural public service campaign in English and Spanish, a wear-a-mask campaign, Latino outreach and a Spanish website.

The CareOregon family’s staff and leaders continue a long-standing role of serving as thought leaders and sharing expertise in the various fields our work touches. We were especially gratified by the Modern Healthcare news organization’s recognizing us for leadership in diversity; CareOregon was among 10 health care organizations nationally to receive this honor. In addition, the respected magazine named President and CEO Eric C. Hunter as one of Top 25 Diversity Leaders in Healthcare. Here’s a sampling of our 68 varied speaking engagements in 2021.
In January, Oyinda Osibanjo, PhD, MPH, RPh and Senior Pharmacy Clinical Coordinator, gave a presentation about vaccine education to this nonprofit, which advocates for low-income Latinas to become community leaders.
Center of Excellence for Integrated Health SolutionsAt a team-based care learning collaborative in March, John Bischof, MD, Medical Director, Behavioral Health, reviewed keys to successfully implementing team-based behavioral health care.
Care Coordination Innovations for Medicaid, Medicare and Dual EligiblesIn August, Keshia Bigler, Director, Network Analytics/Evaluation and Jonathan Weedman, Vice President, Population Health, presented “A case study: The intersection of data, demand and access for the most-complex members.”
Open Minds Management & Best Practices InstituteEric C. Hunter, President and CEO, served as a panelist in August for “Medicaid in the ‘Next Normal:’ Challenges for funding & delivering care for the most-complex consumers” and the related “Thought leader discussion session.”
Oregon Public Health AssociationJames Mason, PhD, Chief Equity, Diversity and Inclusion Officer, gave the keynote at the virtual conference in October. His talk included the tangible benefits of cultural competence for health care organizations.
Business Development InstituteIn October, Amy Dowd, Chief Operations Officer, spoke on, “Know your members? Applying data and analytics to improve health equity.”
CareOregon continued to experience the impact of COVID-19 in 2021. Our membership grew 8% over 2020, as the state paused the redetermination process and — because of the ongoing pandemic — members did not access care at the same level as previous years. CareOregon responded to another difficult year by focusing our efforts on supporting our provider network and community-based organizations that serve our members, donating or pledging more than $19 million and greatly exceeding our past community giving. Through it all, CareOregon remains financially stable and focused on our mission: To inspire and partner to create quality and equity in individual and community health.
511,000
$2.09 billion
$1.10 billion
In the second year of the pandemic, CareOregon concentrated nearly $18 million of community investment in two main areas: our provider networks and community-based organizations.
We prioritized supporting our provider networks’ ability to maintain the vital services they offer our members in seven counties across the state. And we wanted to further the work of community-based organizations that address the factors affecting Oregonians’ health beyond the care they receive from their physical, dental and mental health care providers. These factors, called the social determinants of health, include education, economic stability, neighborhood safety, and social and community supports.

$11,812,235
$4,910,000
$3,210,967
$3,691,268

$2,569,730
$644,100
$486,208
$1,439,422

$3,585,099
$1,275,459
$1,038,876
$1,270,764


Kerry Barnett, JD
Past president and Chief Executive Officer, SAIF
Woody English, MD, MMM
Past president, Housecall Providers
Joanne Fuller, MSW
Retired
(Formerly Multnomah County Health Department)
Tec Han
Chief Investment Officer
Vibrato Capital LLC
Damien R. Hall, Board Chair
Partner
Ball Janik LLP
Susan Hennessy
Retired
(Formerly Kaiser Permanente NW)
Eric C. Hunter
President and Chief Executive Officer
CareOregon
Brenda Johnson
Chief Executive Officer
La Clinica
Nathalie Johnson, MD
Medical Director
Legacy Cancer Services
Andrew McCulloch
Retired
(Formerly Regional President of the Kaiser Foundation Health Plan and Hospitals of the Northwest)
Joined Board December 2021
Gina Nikkel, PhD
Executive Director
Association of Oregon Counties
Suk Rhee
Vice President of Programs
Asian Americans/Pacific Islanders in Philanthropy
Glenn Rodriguez, MD
Retired
(Formerly Providence Milwaukie, Family Medicine Residency Program)
Bob Stewart
Superintendent
Gladstone School District
Nancy Avery
Manager
ODS Community Dental
Jonathan Betlinski, MD, Board Chair
Director, Division of Public Psychiatry
OHSU
Cathy Bond
NW Rides Brokerage Manager
Tillamook County Transportation District
Joined Board July 2021
Pam Cooper
Chief Financial Officer
Providence Seaside Hospital
Sherrie Ford
Director
Columbia Health Services
Henry Heimuller
Commissioner
Columbia County
Tim Hennigan
Medical Services Compliance Officer
Columbia River Fire & Rescue
Joined Board July 2021
Eric C. Hunter
President and Chief Executive Officer
CareOregon
Monica D. Martinez
Vice President/General Counsel, Legal and Regulatory Affairs
CareOregon
Joined Board September 2021
Viviana Matthews
Executive Director
Clatsop Community Action
Debbie Morrow
Community Leader
Warrenton Hammond School District Chair
Marlene Putman
Administrator
Tillamook County Community Health Centers
Bruin Rugge, MD
Associate Professor
Director of Patient Care
OHSU Family Medicine
Erin Skaar
Commissioner
Tillamook County
Eric Swanson
President
Adventist Health Tillamook
Joined Board July 2021
Nicole Williams
Chief Operating Officer
Columbia Memorial Hospital
Laura Bridges, Board Chair
Behavioral Health Officer
La Clinica
John Curtis
Jackson Care Connect
Community Advisory Council
Jason Elzy
Executive Director
Housing Authority of Jackson County
Eric C. Hunter
President and Chief Executive Officer
CareOregon
Brenda Johnson
Chief Executive Officer
La Clinica
Scott Kelly
President and Chief Executive Officer
Asante Health Services
Paul Matz, MD
Rogue Community Health
Cindy Mayo
Retired
(Formerly Chief Executive, Providence, Southern Oregon)
Craig Newton
Co-chair, Jackson Care Connect
Community Advisory Council
William North
Chief Executive Officer
Rogue Community Health
Lori Paris
President and Chief Executive Officer
Addictions Recovery Center
Matt Sinnott
Senior Director
Government Affairs and Contracts
Willamette Dental Group