Your PA Search Just Got a Lot Easier!
One of the questions we frequently receive on the Pharmacy Team is “How do I get this medication approved?” Many drugs on our Oregon Health Plan formulary* have Prior Authorization (PA) criteria that need to be met, so a PA request must be sent to CareOregon. We want to be transparent about the criteria required and the information needed to process these requests. PA criteria have always been posted on the CareOregon website, but we received feedback that it could be hard to navigate – no longer!
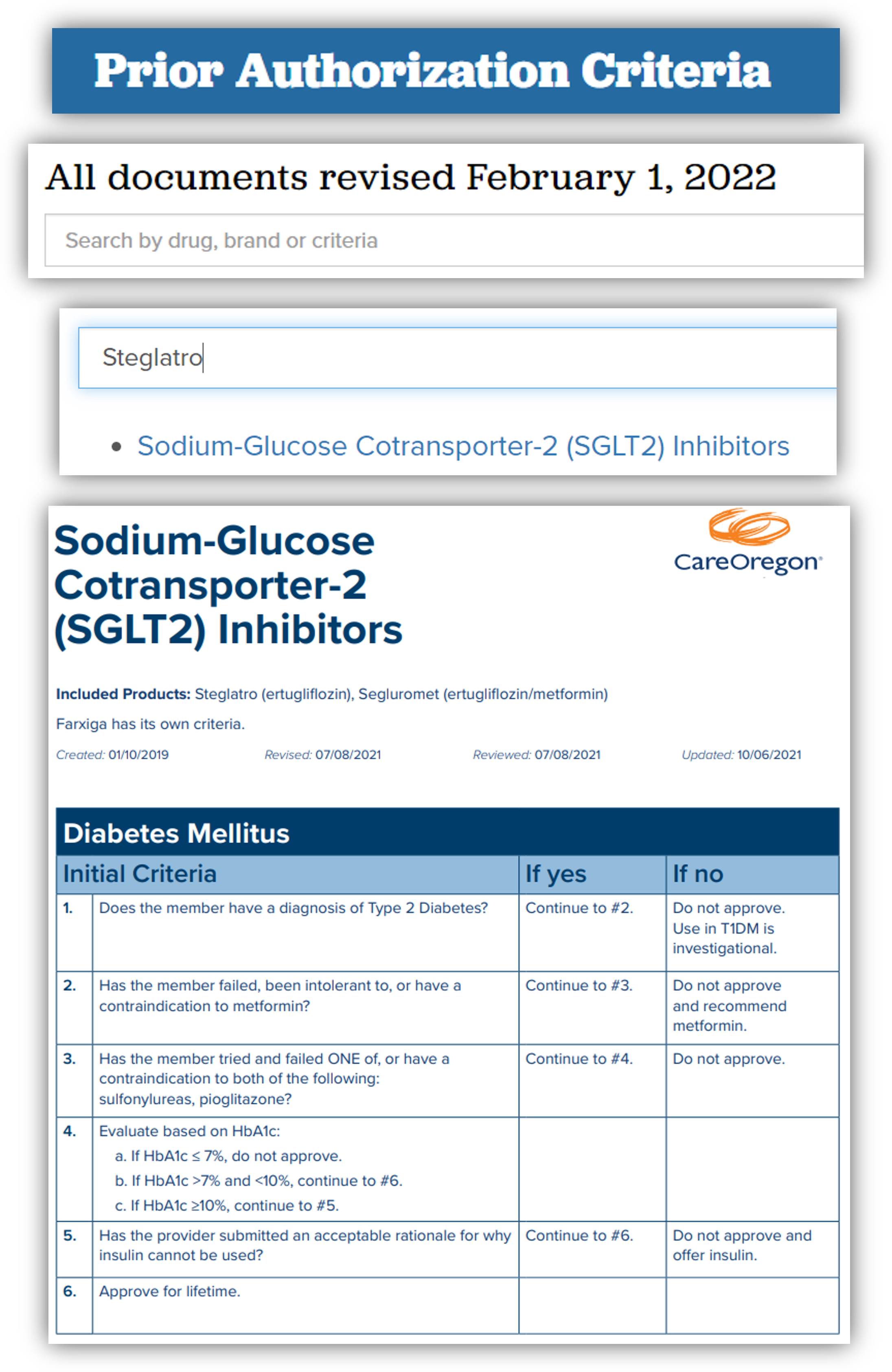
We listened, and we would like to introduce a facelift to our criteria documents and website search tool. The criteria are the same, but we have made it much easier for everyone to use. Instead of one large document, each page is accessible using a new and improved search field. This gets you to exactly where you need with fewer clicks!
Just type what you are looking for: brand name, generic name, or document name – any of these will narrow down the list until you find what you need. The documents themselves have also been reformatted to be easier to read.
We hope that this change will make the PA process easier for everyone, helping you know exactly what information is needed before sending in requests. As always, if you still have questions, our pharmacy staff is just a phone call away!
- Customer Service: 503-416-4100 or 800-224-4840,
- Option 3 for Provider, then Option 3 for Pharmacy Staff.
*Currently applies only to Oregon Health Plan formulary – not CareOregon Advantage.